Introduction
Sterilization is one of the most important steps in any microbiology or medical laboratory. Without proper sterilization, unwanted microorganisms can contaminate samples, affect experimental results, and even spread harmful pathogens.
One of the most widely used sterilization devices is the Autoclave, also known as a steam sterilizer. It uses steam under pressure to kill bacteria, viruses, fungi, and even highly resistant bacterial spores.

Autoclaves are used in:
- Healthcare (sterilizing surgical tools, dressings, and medical waste),
- Microbiology labs (sterilizing glassware, culture media, and instruments),
- Pharmaceutical industries (sterilizing drugs and raw materials),
- Food industries (ensuring microbial safety of food products).
This article explains the principle, parts, types, working, uses, advantages, limitations, and safety precautions of autoclaves in detail.
Principle of Autoclave
- Works on the principle of moist heat sterilization.
- Uses steam under pressure to reach higher temperatures than normal boiling water.
- At 15 psi pressure, water boils at 121°C instead of 100°C.
- This high-pressure steam penetrates materials deeply, ensuring sterilization.
- Steam provides moisture, which causes coagulation and denaturation of proteins, leading to irreversible microbial death.
- Even resistant bacterial spores are destroyed under autoclave conditions.
Standard sterilization conditions:
- 121°C temperature
- 15 psi pressure
- 15–30 minutes (depending on material and load size)
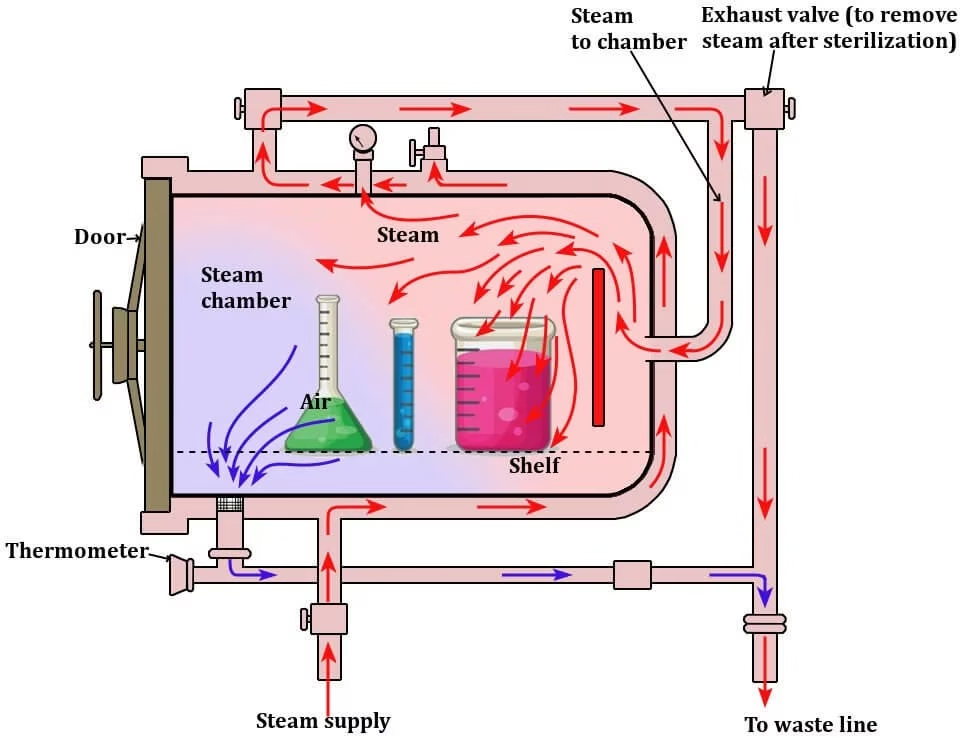
Parts of an Autoclave

Autoclaves come in different sizes and designs, but they generally consist of the following parts:
1. Pressure Chamber
- The main body of the autoclave.
- Made of stainless steel or gunmetal (inner chamber) and an iron case (outer jacket).
- Sizes vary from 100 liters to 3000 liters.
- The outer jacket may be pre-heated with steam to reduce sterilization time.
2. Lid or Door
- Airtight closure with screw clamps and asbestos/rubber washer.
- Prevents leakage and maintains internal pressure.
- Contains:
- Pressure Gauge – shows pressure inside the chamber.
- Safety Valve – releases excess steam if pressure exceeds safe limits.
- Whistle/Release Unit – regulates steam release (similar to a pressure cooker).
3. Steam Generator/Heater
- Electric heater or boiler that produces steam.
- Proper water levels are crucial to avoid damage or improper sterilization.
4. Vacuum Generator (Optional)
- Found in advanced autoclaves.
- Removes air pockets to ensure uniform steam penetration.
5. Wastewater Cooler
- Some autoclaves have a cooling system for hot effluents before disposal.
- Prevents damage to drainage systems.
Working Procedure of an Autoclave
The general steps followed while running an autoclave are:
- Check Chamber – Ensure no leftover material from the previous run.
- Add Water – Place the required amount of water in the chamber.
- Load Materials – Arrange glassware, instruments, or media properly (not overcrowded).
- Seal the Lid – Close and lock the lid tightly.
- Set Parameters – Adjust temperature (121°C), pressure (15 psi), and time (15–30 mins).
- Heating Phase – The heater produces steam, filling the chamber.
- Air Removal – Air escapes through the discharge pipe until only steam remains.
- Sterilization Phase – Pressure and temperature stabilize; sterilization begins.
- Exhaust Phase – After sterilization, heater switches off, pressure decreases gradually.
- Cooling Phase – Wait until pressure gauge shows atmospheric pressure before opening.
- Unload Materials – Carefully remove sterilized items with gloves/tongs.
Types of Autoclaves
- Pressure Cooker Type (N-type)
- Small, simple, and inexpensive.
- Mostly used in teaching labs and small clinics.
- Gravity Displacement Type
- Steam is generated in the chamber itself.
- Most common laboratory autoclave.
- Affordable, but less efficient than advanced types.
- Positive Pressure Displacement Type (B-type)
- Steam generated in a separate steam generator.
- Faster sterilization (steam enters chamber immediately).
- Negative Pressure Displacement Type (S-type)
- Equipped with both steam generator and vacuum pump.
- Removes air completely, ensures uniform sterilization.
- Highly reliable but also expensive.

Uses of Autoclave
- Sterilization of culture media, glassware, and instruments.
- Decontamination of medical waste before disposal.
- Sterilizing surgical instruments in hospitals.
- Sterilizing autoclavable plastic items (pipette tips, tubes, containers).
- Pharmaceutical industry – sterilizing raw materials, dressings, solutions.
- Food industry – ensuring safety of canned and packaged foods.
Advantages of Autoclave
- Kills all types of microorganisms including spores.
- Faster and more effective than dry heat sterilization.
- Safe and economical for large-scale use.
- Can sterilize liquids, solids, instruments, and medical waste.
- Provides reproducible results with proper monitoring.
Limitations of Autoclave
- Cannot sterilize oils, powders, or heat-sensitive materials.
- Items like plastics may melt if not autoclavable.
- Requires careful handling to avoid burns and accidents.
- Expensive models (vacuum-based) may not be affordable for small labs.
- Requires electricity and water supply.
Precautions While Using an Autoclave
- Do not overload the chamber.
- Ensure items are autoclavable before use.
- Use only autoclavable bags for waste.
- Do not autoclave flammable, corrosive, or toxic materials.
- Always wait for pressure to normalize before opening.
- Liquids should not be sealed completely (risk of explosion).
- Load liquids only up to 2/3rd of the container volume.
- Wear gloves and lab coat when unloading sterilized items.
Applications in Different Fields
- Medical Labs: Sterilization of surgical tools, dressings, medical waste.
- Microbiology Labs: Sterilizing culture media, instruments, and glassware.
- Pharmaceutical Industry: Sterilizing drugs, IV fluids, and equipment.
- Food Industry: Sterilizing canned foods, testing microbial contamination.
- Research: Ensuring sterile conditions for molecular biology, biotechnology, and genetics experiments.
Frequently Asked Questions (FAQ)
Q1. What is the working temperature and pressure of an autoclave?
Standard conditions are 121°C at 15 psi for 15–30 minutes.
Q2. What items cannot be sterilized in an autoclave?
Oils, powders, flammable materials, plastics not labeled as autoclavable.
Q3. Why is autoclaving better than dry heat sterilization?
Because moist heat penetrates deeper and kills microbes faster than dry heat.
Q4. What is the most advanced type of autoclave?
The negative pressure displacement autoclave (S-type) is the most advanced and reliable.
Q5. Why should we not open an autoclave immediately after sterilization?
Because high pressure and temperature can cause burns and accidents. Wait until pressure is back to normal.
References
- Frazier WC and Westhoff DC. Food Microbiology. Tata McGraw Hill Publishing Company Limited. 1995.
- Banwart GJ (1989). Basic Food Microbiology. Chapman & Hall, New York, NY.
- Jay JM (2000). Modern Food Microbiology. CBS Publications and Distribution. Delhi.
- Collins CH, Patricia M, and Lyne JM (1995). Collins and Lynes Microbiological Methods 7th edition. Grange, Butter Worth, Oxford.
- Cappucino JG and Sherman N (1996). Microbiology, A Laboratory Manual 4th edition. Benjamin Cumings Inc. California
- https://microbenotes.com/autoclave/
- https://www.researchgate.net/publication/242234753_Design_and_Construction_of_an_Autoclave
Other related topics you might be interested in:
Autoclave – Principle, Parts, Procedure, Types, Uses, Advantages, Limitations
Bioreactor – Principle, Design, Parts, Types, Applications, and Limitations
Bunsen Burner – Principle, Parts, Types, Flames, Applications, Advantages & Precautions
Centrifuge – Principle, Parts, Types, Operation, Applications and Advantages
Hot Air Oven – Principle, Parts, Types, Working, Applications & Advantages
Instruments Used in Microbiology Laboratory – Principles, Uses, and Applications
Laboratory Incubator – Principle, Types, Components, Working, Applications, Advantages & Limitations
Laminar Flow Hood / Cabinet – Principle, Types, Parts, Procedure, Applications & Precautions
pH Meter – Principle, Parts, Working, Procedure, Types, Applications, Advantages & Precautions
Pipettes – Principle, Types, Uses, Parts, Operation, Advantages & Precautions